Before becoming a Cavalier King Charles Spaniel parent, I was unaware of their genetic issues. So before I started to look for a puppy to adopt into the family, I thought it was necessary to look for the most common genetic defects in a Cavalier. Here is what I discovered.
- Mitral valve disease (MVD)
- Chiari-like malformation (CM)
- Syringomyelia (SM)
- Primary secretory otitis media (PSOM), aka glue ear
- Episodic falling syndrome (EFS)
- Curly coat syndrome
- Dry eye syndrome
- Diabetes mellitus
- Patellar luxation
It’s not enough to just know the names of the problems; if you plan to become a Cavalier parent, you must know the details of each disorder to be fully prepared. Read on to learn more about the most common genetic defects in a Cavalier.
1. Mitral Valve Disease (MVD)
Mitral Valve Disease (MVD) is a prevalent health issue among Cavalier King Charles Spaniels, accounting for many ill health cases and deaths worldwide. This chronic condition adversely impacts heart function and threatens our beloved pets’ well-being.
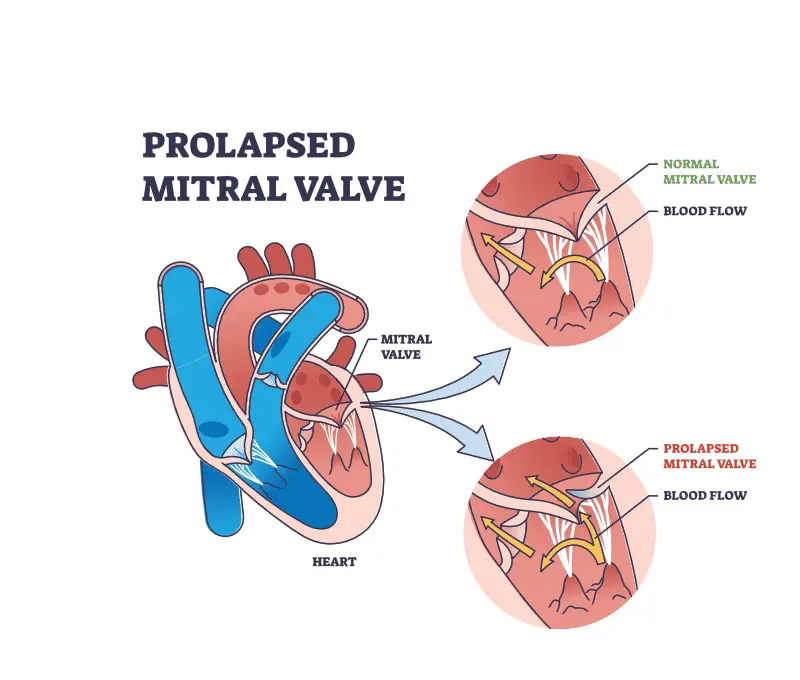
The mitral valve plays a crucial role in maintaining proper blood flow within the heart. However, when MVD develops, this valve degenerates, causing issues such as heart murmurs and eventually congestive heart failure in severe cases.
The mitral valve’s primary function is to ensure that blood flows in one direction, from the left atrium to the left ventricle.
In MVD, the mitral valve becomes thickened, distorted, and less flexible over time, leading to a progressive leakage of blood backward from the left ventricle into the left atrium.
This condition is known as mitral regurgitation. As the disease progresses, the regurgitation worsens, causing enlargement of the left atrium and, eventually, the left ventricle. At this point, it can lead to congestive heart failure and other related complications.
What Causes MVD?
The exact cause of MVD is not fully understood, but it is believed to be multifactorial, involving genetic and environmental factors.
Cavaliers have a particularly high prevalence of MVD compared to other dog breeds, with some studies suggesting a genetic predisposition and possibly other factors, such as age and sex, contributing to the disease’s progression.
MVD Symptoms and Diagnosis
Symptoms of MVD can vary depending on the severity of the condition. In the early stages, dogs may not exhibit any noticeable signs.
As the disease progresses, symptoms may include coughing, difficulty breathing, fatigue, exercise intolerance, decreased appetite, weight loss, and even fainting or collapse in severe cases.
Diagnosing MVD typically involves a combination of physical examination, medical history review, and diagnostic tests. The veterinarian may listen to the dog’s heart using a stethoscope to detect abnormal heart sounds or murmurs.
Additional tests such as chest X-rays, electrocardiogram (ECG), echocardiography (ultrasound of the heart), and blood tests may be performed to assess the severity of the disease, evaluate cardiac function, and rule out other possible causes of the symptoms.
Treating MVD
While there is no cure for MVD, the treatment aims to manage the symptoms, slow the disease progression, and improve the dog’s quality of life. Medications such as diuretics, ACE inhibitors, and a medication known as pimobendan may be prescribed to reduce fluid accumulation, lower blood pressure, and enhance heart function.
Regular follow-up visits with the veterinarian are necessary to monitor the dog’s condition and adjust the treatment.
In advanced stages of MVD, when congestive heart failure develops, more intensive treatments, such as oxygen therapy, hospitalization, and in some cases, surgical interventions, may be considered. Surgical options include valve repair or replacement, but these are complex procedures typically performed by specialized veterinary cardiac surgeons.
It is important for Cavvys to undergo regular cardiac screenings and other recommended tests, even in the absence of symptoms. Early detection and intervention can help manage the disease more effectively and improve the long-term prognosis.
2. Chiari-like Malformation (CM)
Chiari-like malformation (CM) is a structural abnormality affecting the skull and brain, particularly in small breed dogs such as Cavaliers. It is characterized by a mismatch between the size of the brain and the size of the skull, leading to compression and herniation of brain tissue into the spinal canal.
In CM, the back of the skull, known as the occipital bone, is too small or abnormally shaped. This results in a constricted space within the skull, causing overcrowding of the brain structures at the base of the skull, including the cerebellum and brainstem.
The herniation of these structures into the spinal canal through the opening at the back of the skull is called syringomyelia (explained below).
What Causes CM?
The exact cause of CM is not fully understood, but it is believed to have a genetic component. It is thought to be inherited from one parent to develop the condition. Other factors, such as environmental and developmental influences, may also contribute to the severity of CM.
Cavalier King Charles Spaniels have a particularly high prevalence of CM compared to other breeds, with estimates suggesting that over 90% of the breed is affected. However, it is important to note that not all Cavaliers with CM will develop clinical signs.
CM Symptoms and Diagnosis
The compression and herniation of brain tissue in CM can lead to a range of symptoms. The most common and notable symptom is nerve pain, which is typically characterized by episodes of intense, burning pain in the neck, shoulders, and limbs.
Cavvys may start scratching or rubbing the area, head shaking, yelping, and reluctance to be touched or have their necks handled. Other signs include abnormal walking, weakness, limb paralysis, wasting muscle mass, and changes in their behavior.
Diagnosing CM involves a combination of tests, such as examination of the nervous system and diagnostic imaging.
Magnetic resonance imaging (MRI) is the main way of detecting and assessing the severity of CM and associated syringomyelia, as it allows for the visualization of the brain, skull, and spinal cord to determine the extent of herniation.
Treating CM
While there is no cure for CM, treatment aims to manage the clinical signs and improve the dog’s quality of life.
Medications such as pain relievers, anti-inflammatory drugs, and drugs that help the flow of spinal fluid may be prescribed to alleviate pain, reduce inflammation, and manage fluid buildup.
Physical therapy, including exercises and massage, can also help improve muscle strength and mobility.
In severe cases of CM, surgery may be considered.
Surgical options include decompression surgery, where a portion of the skull is removed to alleviate pressure on the brain and spinal cord, and shunt placement to redirect the flow of spinal fluid.
Ultimately, responsible breeding practices are crucial in reducing the prevalence of CM in Cavaliers. Breeders should aim to selectively breed dogs without CM and promote the welfare of future generations.

3. Syringomyelia (SM)
Syringomyelia is the formation of fluid-filled cavities called syrinxes within the spinal cord and is commonly associated with Chiari-like malformation (see above).
Due to the high probability of being born with CM, Cavaliers are particularly prone to developing syringomyelia too.
The overcrowding and compression of brain structures at the base of the skull prevent the spinal fluid from flowing freely. As a result, the fluid accumulates and forms fluid-filled cavities or syrinxes within the spinal cord.
The syrinxes can extend and expand along the length of the spinal cord, causing damage to the surrounding nerve tissue.
What Causes SM
The exact mechanisms of syrinx formation and progression are not fully understood, but it is believed that the altered spinal fluid flow, pressure changes, and fluid accumulation contribute to the development and size increase of syrinxes.
SM Symptoms and Diagnosis
The most common symptom is nerve pain, typically involving the neck, shoulders, and limbs.
Your Cavvy may start scratching, rubbing, or biting the area, aimed at relieving the discomfort.
Other signs that are the same with CM may include weakness, limb paralysis, wasting muscle mass, difficulty walking, behavioral changes, and even an altered sensation.
Diagnosing syringomyelia involves a combination of clinical checks, nerve examinations, and MRI scans. Pretty much the same diagnosis as CM.
Treating SM
Similar to CM, the aim is to manage pain and improve the dog’s quality of life.
Medications such as pain relievers, anti-inflammatory drugs, and drugs that promote the flow of spinal fluid may be prescribed.
Massage and exercise can also be beneficial in improving muscle strength and mobility. Again, in severe cases of syringomyelia, surgery may be considered.
4. Primary Secretory Otitis Media (PSOM)
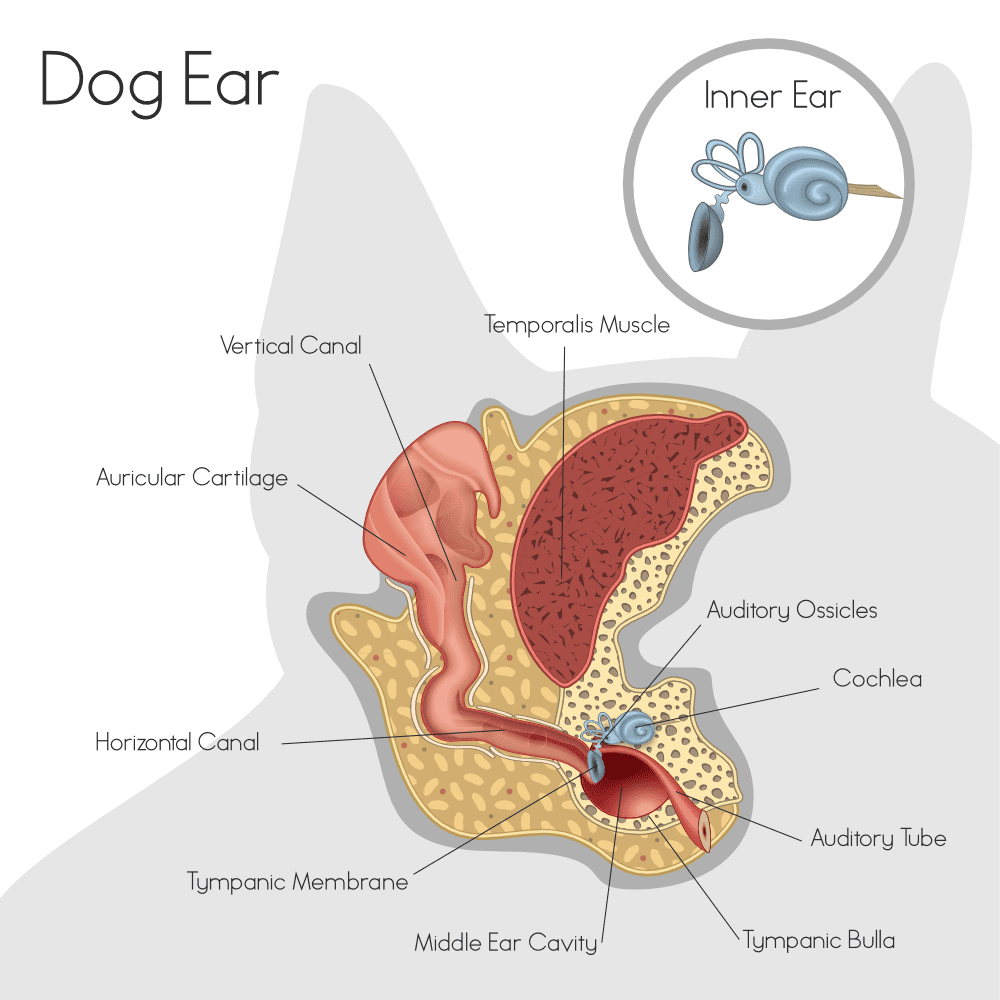
Primary secretory otitis media (PSOM), also known as “glue ear” or “middle ear effusion,” is a condition that affects the middle ear of dogs, particularly Cavalier King Charles Spaniels.
It is distinguished by the accumulation of thick, sticky mucus-like fluid in the middle ear cavity, leading to hearing loss and other related symptoms.
In a healthy ear, the middle ear contains air and is connected to the back of the throat through a narrow tube called the Eustachian tube.
This tube helps equalize the pressure in the middle ear and drain any fluid or mucus that may accumulate. However, in Cavvys with PSOM, the Eustachian tube becomes obstructed, preventing the proper drainage of fluid.
What Causes PSOM
The exact cause of PSOM is not fully understood, but it is believed to be a combination of genetic and anatomical factors.
Cavalier King Charles Spaniels have been found to have a higher prevalence of PSOM compared to other breeds, suggesting a possible genetic predisposition. The structure of their skull, particularly the shape and size of the tympanic bulla (a bony chamber that houses the middle ear), may also contribute to the development of PSOM.
PSOM Symptoms and Diagnosis
The accumulation of mucus-like fluid in the middle ear causes various symptoms, including hearing loss, head shaking, scratching or pawing at the ears, pain or discomfort, and balance problems.
Some dogs may also exhibit signs of ear infection, such as redness, swelling, and discharge from the ear.
Diagnosing PSOM typically involves a thorough examination of the dog’s ears using an otoscope, which allows the veterinarian to visualize the middle ear.
The characteristic finding is the presence of thick, glue-like fluid that obstructs the view of the middle ear structures. In some cases, further diagnostic tests such as computed tomography (CT) or magnetic resonance imaging (MRI) may be necessary to confirm the diagnosis and assess the severity of the condition.
Treating PSOM
The treatment of PSOM usually involves the removal of the accumulated fluid from the middle ear. This is typically done under general anesthesia, as it requires the insertion of a small catheter or needle through the eardrum to drain the fluid.
Sometimes, a ventilation tube may be placed in the eardrum to help maintain airflow and prevent fluid accumulation. Additionally, if there is evidence of infection, appropriate antibiotics or other medications may be prescribed.
It is important to note that while the treatment can provide temporary relief, PSOM has the potential to recur. Some dogs may require repeated drainage procedures or long-term management to control the condition.
Regular monitoring by a veterinarian is essential to ensure the dog’s comfort and overall ear health.
5. Episodic Falling Syndrome (EFS)
Episodic Falling Syndrome (EFS) is a genetic disorder that affects the skeletal muscles of dogs, particularly Cavalier King Charles Spaniels.
It is characterized by episodes of muscle stiffness and involuntary contractions, leading to an inability to walk or stand. The condition is believed to be caused by a mutation in a specific gene known as BCAN (brevican).
During an episode of EFS, affected dogs experience sudden muscle stiffness and rigidity, often triggered by excitement, stress, or exercise.
The stiffness affects the muscles of the limbs and trunk. As a result, the affected Cavvy may assume a rigid, extended posture, with the limbs held straight out and the back arched. They are unable to move, walk, or stand, despite their attempts to do so.
These episodes typically last a few minutes to several hours before the dog recovers and returns to normal.
What Causes EFS
EFS is inherited from the parents and is known as autosomal recessive, meaning an affected dog must inherit a copy of the mutated gene from both parents to develop the condition.
Dogs that carry only one copy of the mutation are considered carriers and do not exhibit clinical signs.

EFS Symptoms and Diagnosis
Diagnosing EFS involves a combination of clinical assessments, a medical history review, and genetic testing.
During an episode, the characteristic rigid posture and the dog’s inability to move or walk are typical of the condition. Genetic testing can confirm the presence of the BCAN mutation and determine whether a dog is affected, a carrier, or clear of the mutation.
Treating EFS
There is no cure for EFS, but affected Cavvys can still lead a relatively normal life with the appropriate management.
When it happens, it is essential to keep the dog calm and avoid further stimulation, as stress or exercise can exacerbate the symptoms. Some dogs may benefit from gentle massage or stretching to help relieve muscle tension.
In severe cases, medications such as anti-seizure drugs or muscle relaxants may be prescribed to reduce the frequency and severity of each episode.
Breeders play a crucial role in preventing the spread of EFS by implementing responsible breeding practices. Genetic testing should be performed to identify carriers and avoid breeding them to other carriers, as this increases the risk of producing puppies affected by the disorder.
6. Curly Coat Syndrome (CCS)
Curly Coat Syndrome is a disorder characterized by a curly, wiry, and excessively thick coat in affected dogs, and is also known as rough coat.
Dogs with CCS typically exhibit abnormal hair texture and growth patterns from an early age.
The curly coat in affected Cavvys may be present all over the body or localized to certain areas. The hair can be tightly curled, dense, and difficult to groom.
What Causes CCS
The condition is caused by a mutation in the FGF5 (fibroblast growth factor 5) gene, which plays a role in hair growth and development.
CCS Symptoms and Diagnosis
To diagnose CCS, a genetic test can be performed to detect the presence of the FGF5 mutation. The test can identify whether a dog is clear (not carrying the mutation), a carrier (carrying one copy of the mutation), or affected (carrying two copies of the mutation).
Treating CCS
Sometimes, it may lead to hair loss or patchy coat patterns, but the primary symptom is related to the coat.
When Cavvy puppies grow into adults, their skin may deteriorate, causing them to feel extremely uncomfortable, and therefore will need a lifetime of daily medicated baths to treat the skin.

7. Dry Eye Syndrome
Dry Eye Syndrome, also known as Keratoconjunctivitis sicca (KCS), is a condition characterized by insufficient tear production or poor tear quality, leading to dryness and inflammation of the eyes.
It can affect various dog breeds, including Cavalier King Charles Spaniels, although it is not specific to this breed.
Tears play a crucial role in maintaining the health and lubrication of the eyes. They provide moisture, nutrients, and protection against foreign particles and infections.
In dogs with Dry Eye Syndrome, there is a deficiency in tear production or an imbalance in the components of tears, leading to inadequate lubrication of the eyes.
What Causes Dry Eye Syndrome
The exact cause of Dry Eye Syndrome in dogs, including Cavaliers, can vary. Here are a few possibilities;
- Immune-mediated Response, where the immune system mistakenly attacks and damages the tear-producing glands.
- Specific medications
- Infections
- Underlying Diseases
- Inherited Abnormalities
- Trauma to the Eyes
Dry Eye Symptoms and Diagnosis
The primary symptom of Dry Eye Syndrome is dryness and irritation of the eyes.
Affected Cavaliers may exhibit redness, squinting, increased blinking, discharge from the eyes, and discomfort.
In some cases, the lack of tear production can lead to corneal ulcers or erosions, which can cause pain and further complications if left untreated.
To diagnose Dry Eye Syndrome, a veterinarian will perform a thorough examination of the eyes, including evaluating tear production. A test called the Schirmer tear test is commonly used to measure the amount of tear production.
It involves placing a small strip of special paper in the lower eyelid to absorb tears over a specified time. If tear production is significantly reduced, it indicates Dry Eye Syndrome.

Treating Dry Eye Syndrome
The treatment of Dry Eye Syndrome aims to increase tear production, relieve discomfort, and prevent any further complications.
The initial treatment uses artificial tears or lubricating ointments to provide moisture and improve eye lubrication. These products need to be applied regularly throughout the day.
In cases where tear production is severely lacking, additional medical interventions may be necessary. Immunosuppressive medications to suppress the immune system can be prescribed to reduce inflammation and improve tear production.
These medications typically need to be used long-term to manage the condition effectively.
Regular monitoring by yourself and a veterinarian is crucial to assess tear production, monitor the dog’s response to treatment, and adjust the management plan if necessary. Although Dry Eye Syndrome cannot be cured, managing it can significantly improve your Cavvys comfort and minimize the risk of complications.
8. Diabetes Mellitus
Diabetes Mellitus is a metabolic disorder characterized by elevated blood glucose levels due to insufficient insulin production or ineffective utilization of insulin.
Although suffered by humans, Cavaliers, and all dog breeds suffer from it too. It is especially close to me as our Cavalier, Lady, suffers from it too.
The insulin hormone produced by the pancreas helps regulate blood sugar levels and allows cells to use glucose for energy. When the body cannot properly regulate blood glucose levels, it leads to the development of diabetes.
There are two main types of diabetes in dogs: Type 1 and Type 2. The same as humans.
Type 1 diabetes occurs when the pancreas fails to produce enough insulin.
Type 2 diabetes, on the other hand, is characterized by the body’s inability to use insulin effectively, known as insulin resistance. Dogs primarily develop Type 1 diabetes.
What Causes Diabetes Mellitus
While diabetes can affect dogs of any breed, Cavalier King Charles Spaniels are among the breeds that have been found to have a higher predisposition to the condition. The exact reason for this increased susceptibility in Cavaliers is not yet fully understood, but it is believed to have a genetic component.
Diabetes Mellitus Symptoms and Diagnosis
In dogs with diabetes, the inability to regulate blood glucose levels leads to increased levels of glucose in the bloodstream, resulting in hyperglycemia. The excess glucose is then excreted through urine, causing increased urination and excessive thirst (polyuria and polydipsia, respectively). Dogs with diabetes often exhibit increased appetite (polyphagia) as well, as the body is unable to utilize glucose efficiently for energy.
Other common symptoms of diabetes in dogs include weight loss, lethargy, cloudy eyes (due to cataract formation), urinary tract infections, and a weakened immune system. If left untreated, diabetes can lead to more severe complications, such as diabetic ketoacidosis, which is a life-threatening condition characterized by the accumulation of ketones in the blood.
Diagnosing diabetes involves a combination of clinical signs, blood tests, and urine tests. A veterinarian will evaluate the dog’s symptoms and perform blood tests to measure blood glucose levels. Persistent hyperglycemia, along with the presence of glucose in the urine (glucosuria), confirms the diagnosis of diabetes.
Treating Diabetes Mellitus
The primary goal of diabetes management is to regulate blood glucose levels and minimize symptoms. Treatment typically involves insulin therapy, where injections are administered to replace deficient or ineffective insulin.
The specific insulin type, dosage, and frequency are determined based on the individual dog’s needs and response to treatment.
Monitoring blood glucose levels at home using a glucometer and working closely with a veterinarian to adjust the treatment plan is essential for effective management.
Our vet suggested trying a Freestyle Libre sensor so that we could scan Lady more frequently over a two-week period, as pricking her ear every two hours would cause her too much discomfort.
The results were incredible and was able to get her to the right level of insulin required. Don’t get me wrong; it’s not that simple. It’s taken over 10 months of trial and error to get her to a comfortable level of insulin for her diabetes.

The diet also plays a crucial role in managing diabetes in dogs. A balanced and consistent diet, with appropriate carbohydrate levels and a regular feeding schedule, helps regulate blood glucose levels.
Prescription diets specifically formulated for diabetic dogs may be recommended, or a low-fat diet. Regular exercise is also beneficial for maintaining healthy body weight and improving insulin sensitivity.
9. Patellar Luxation
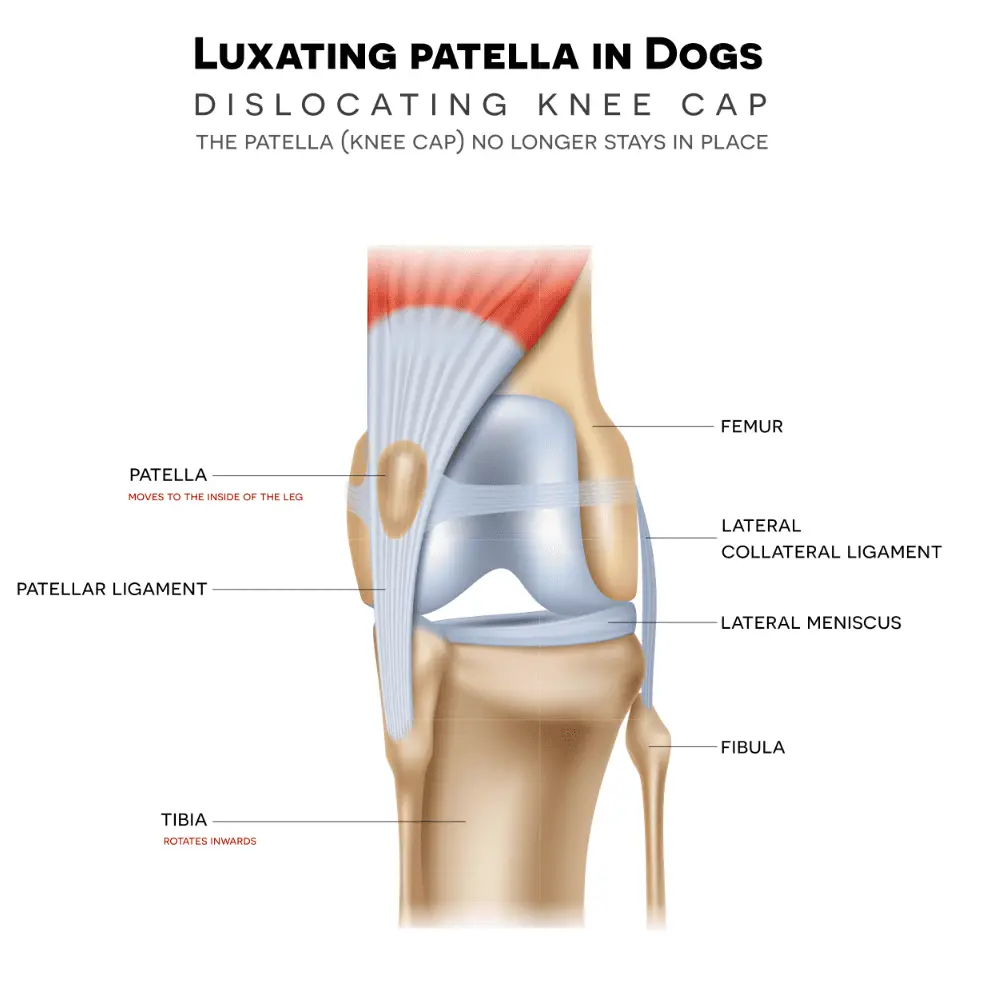
Patellar luxation, also known as kneecap dislocation, is a condition where the kneecap (patella) moves out of its normal position within the groove of the thigh bone (femur). This misalignment can lead to varying degrees of lameness and discomfort.
The patella is an important structure that helps with the movement of the knee joint. It slides within the femoral groove as the leg flexes and extends.
In dogs with patellar luxation, the groove may be shallow or malformed, or the surrounding soft tissues and ligaments may be weak or poorly developed. These factors can contribute to the kneecap’s instability and displacement.
Patellar luxation is classified into different grades based on the severity:
- Grade 1: The patella can be manually luxated but spontaneously returns to its normal position.
- Grade 2: The patella can be manually luxated and remains displaced until manually repositioned.
- Grade 3: The patella is permanently luxated but can be manually repositioned.
- Grade 4: The patella is permanently luxated and cannot be manually repositioned.
What Causes Patellar Luxation
Cavaliers are genetically predisposed to patellar luxation, which is believed to be inherited, although the exact mode of inheritance is not fully understood.
Other factors that may contribute to patellar luxation include conformational abnormalities, such as a shallow femoral groove or abnormal alignment of the bones in the leg.
Patellar Luxation Symptoms and Diagnosis
Symptoms of patellar luxation can vary depending on the severity and grade of the condition. Cavvys may exhibit any of the following;
- Intermittent lameness
- Reluctance to put weight on the affected leg
- Skipping or hopping
- Sudden leg movements to reposition the patella
In more severe cases, dogs may experience constant lameness and discomfort.
Diagnosing patellar luxation involves a physical examination by a veterinarian. The vet will manipulate the patella to assess its stability and determine the grade of luxation.
X-rays may also be taken to evaluate the knee joint and assess any underlying skeletal abnormalities.
Treating Patellar Luxation
Treatment depends on the severity of the condition and the impact it has on the dog’s quality of life. In mild cases where the luxation is infrequent and does not cause significant discomfort, pain management may be recommended.
This typically involves monitoring the dog’s condition, managing the pain or inflammation, and providing regular exercise to maintain muscle strength and joint stability.
In more severe or persistent cases, surgery may be necessary.
Postoperative rehabilitation, including controlled exercise, physical therapy, and weight management, is important for a successful recovery and long-term joint health.

